Shoulder impingement syndrome is a condition where your shoulders rotator cuff tendons are intermittently trapped and compressed during shoulder movements This causes injury to the shoulder tendons and bursa resulting in painful shoulder movements.
Impingement (impact on bone into the rotator cuff tendon or bursa) should not occur during normal shoulder function. When it does happen, the rotator cuff tendon becomes inflamed and swollen, a condition called rotator cuff tendonitis. Likewise if the bursa becomes inflamed, shoulder bursitis will develop.
Both these conditions can co-exist or be present independently.
While a traumatic injury can occur eg fall, it is repeated movement of your arm into the impingement zone overhead that most frequently causes the rotator cuff to contact the outer end of the shoulder blade (acromion). When this repeatedly occurs, the swollen rotator cuff is trapped and pinched under the acromion.
Injuries vary from mild tendon inflammation (tendonitis), bursitis (inflammed bursa), calcific tendonitis (bone forming within the tendon) through to partial and full thickness rotator cuff tendon tears, which may require surgery.
What Causes Shoulder Impingement?
The shoulders rotator cuff tendons are protected from simple knocks and bumps by bones (mainly the acromion) and ligaments that form a protective arch over the top of your shoulder.
In between the rotator cuff tendons and the bony arch is the subacromial bursa (a lubricating sack), which helps to protect the tendons from touching the bone and provide a smooth surface for the tendons to glide over.
However, nothing is foolproof. Any of these structures can be injured, whether they be your bones, muscles, tendons, ligaments or bursas.
Shoulder impingement has primary (structural) and secondary (posture & movement related) causes.
Primary Rotator Cuff Impingement – Structural Narrowing
Some of us are born with a smaller sub-acromial space. Conditions such as osteoarthritis can also cause the growth of sub-acromial bony spurs, which further narrows the space.
Because of this structural narrowing, you are more likely to squash, impinge and irritate the soft tissues in the sub-acromial space, which results in bursitis or shoulder tendonitis.
Secondary Rotator Cuff Impingement – Dynamic Instability
Impingement can occur if you have a dynamically unstable shoulder. This means that there is a combination of excessive joint movement, ligament laxity and muscular weakness around the shoulder joint. This impingement usually occurs over time due to repetitive overhead activity, trauma, previous injury, poor posture or inactivity.
In an unstable shoulder, the rotator cuff has to work harder, which can cause injury. An overworking rotator cuff fatigues and eventually becomes inflamed and weakens due to pain inhibition or tendon tears.
When your rotator cuff fails to work normally, it is unable to prevent the head of the humerus (upper arm) from riding up into the sub-acromial space, causing the bursa or tendons to be squashed.
Failure to properly treat this instability causes the injury to recur. Poor technique or bad training habits such as training too hard is also a common cause of overuse injuries, such as bursitis or tendonitis.
What are the Symptoms of Shoulder Impingement?
Commonly rotator cuff impingement has the following symptoms:
- An arc of shoulder pain approximately when your arm is at shoulder height and/or when your arm is overhead.
- Shoulder pain that can extend from the top of the shoulder to the elbow.
- Pain when lying on the sore shoulder.
- Shoulder pain at rest as your condition deteriorates.
- Muscle weakness or pain when attempting to reach or lift.
- Pain when putting your hand behind your back or head.
- Pain reaching for the seat-belt.
Who Suffers Shoulder Impingement?
Impingement syndrome is more likely to occur in people who engage in physical activities that require repeated overhead arm movements, such as tennis, golf, swimming, weight lifting, or throwing a ball.
Occupations that requires repeated overhead lifting or work at or above shoulder height are also at risk of rotator cuff impingement.
How is Shoulder Impingement Diagnosed?
Shoulder impingement can be diagnosed within the clinic by your physiotherapist or osteopath.
Ultrasound scan may be useful to visualise dynamic impingement and detect associated any associated injuries such as shoulder bursitis, rotator cuff tears, calcific tendonitis or shoulder tendinopathies.
During your ultrasound scan the sonographer or radiologist can visualise what is happening as your shoulder moves through the impingement zone.
What is the Shoulder Impingement Zone?
Postures that significantly narrow the subacromial space are:
- Your arm directly overhead such as plasterers or electricians.
- Your arm working at or near shoulder height.

Who Suffers Shoulder Impingement Syndrome?
Impingement syndrome is more likely to occur in people who engage in physical activities that require repeated overhead arm movements, such as tennis, golf, swimming, weight lifting, or throwing a ball.
Occupations that requires repeated overhead lifting or work at or above shoulder height are also at risk of rotator cuff impingement.
Shoulder Impingement Treatment
There are many structures that can be injured in rotator cuff impingement. How the impingement occurred is the most important question to answer. This is especially important if the onset was gradual since your static and dynamic posture, muscle strength, flexibility and spine shape all have important roles to play.
Once you suspect any rotator cuff injury, it is important to confirm the exact type of your rotator cuff injury since treatment does vary depending on the specific or combination of rotator cuff injuries.
Your rotator cuff is an important group of control and stability muscles that maintain “centralisation” of your shoulder joint. In other words, it keeps the shoulder ball centred over the small socket. This prevents injuries such as impingement, subluxations and dislocations.
We also know that your rotator cuff provides subtle glides and slides of the ball joint on the socket to allow full shoulder movement. Plus, your shoulder blade (scapula) has a vital role as the main dynamically stable base plate that attaches your arm to your chest wall.
Researchers have concluded that there are essentially 7 stages that need to be covered to effectively rehabilitate these injuries and prevent recurrence.
These are:
- Early Injury: Protection, Pain Relief & Anti-inflammatory Treatment
- Regain Full Shoulder Range of Motion
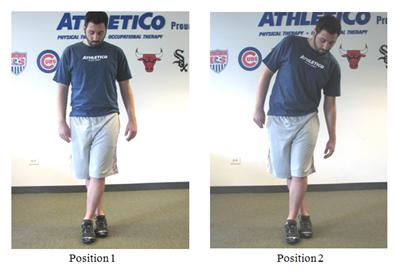
- Restore Scapular Control and Scapulohumeral Rhythm
- Restore Normal Neck-Scapulo-Thoracic-Shoulder Function
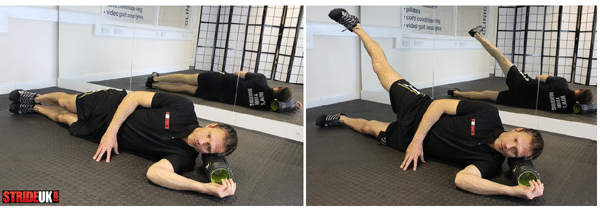
- Restore Rotator Cuff Strength
- Restore High Speed, Power, Proprioception and Agility Exercises
- Return to Sport or Work
For more specific advice about your shoulder impingement, please contact your osteopath.
Corticosteroid Injections
Corticosteroid injections can be useful in the initial pain relieving stage if conservative methods fail to reduce the pain and inflammation. It is important to note that once you pain settles, it is important to assess your strength, flexibility, neck and thoracic spine involvement plus your scapulohumeral rhythm to ensure that your shoulder impingement does not return once your injection has worn off.
How Long Does is Your Recovery?
Every shoulder impingement is different. Some impingements will respond positively to one treatment session, whereas a more complicated case may take many weeks or a few months to settle. Others may require shoulder surgery.
There is no specific time frame for when to progress from each stage to the next. Your injury rehabilitation status will be determined by many factors during your physiotherapist’s clinical assessment.
You’ll find that in most cases, your osteopath will seamlessly progress between the rehabilitation phases as your clinical assessment and function improves.It is also important to note that each progression must be carefully monitored as attempting to progress too soon to the next level can lead to re-injury and frustration.
For more specific advice about your shoulder impingement, please contact www.rotheryhealth.com or call 07951381265